Aiming High: The Strategy for USP Compliance Success
.png?width=1240&height=413&name=Aiming%20High%20The%20Strategy%20for%20USP%20Compliance%20Success%20(2).png)
Vital changes to USP regulations impact Compounding Pharmacies
Handling potentially hazardous drugs is a part of life for healthcare personnel, but what does that look like from a risk perspective?
Healthcare workers are regularly exposed to hundreds of different types of potentially harmful drugs.
From a workplace safety perspective, there has long been an awareness of the need to codify the safety of the environment for the well-being of healthcare professionals.
As a result, the National Institute for Occupational Safety and Health (NIOSH) has established definitive criteria and identified these hazardous drugs.
In concert with the United States Pharmacopeia (USP), they have established comprehensive standards governing the handling of such drugs, with the aim of minimizing risk to public health, according to the USP.
The National Institute for Occupational Safety and Health (NIOSH) refers to a drug as hazardous if it exhibits one or more of the following characteristics in humans or animals:
-
- Carcinogenicity
- Teratogenicity or developmental toxicity
- Reproductive toxicity
- Organ toxicity at low doses
- Genotoxicity
- Structure and toxicity profiles of new drugs that mimic existing hazardous drugs
The United States Pharmacopeia – National Formulary (USP-NF) includes over 5,000 quality standards for medicines, both chemical and biologic; active pharmaceutical ingredients (APIs); and excipients (inactive ingredients).
It is considered the most comprehensive source for medicine quality standards.
The standards crafted by the USP serve multiple purposes:
-
- Enhancing awareness regarding the potential dangers associated with handling hazardous drugs
-
- Providing uniform and standardized guidance, minimizing the inherent risks involved in managing such substances
-
- Reducing the overall risk posed to both patients and the broader healthcare workforce
The collaborative efforts of NIOSH and USP are pivotal in fostering a safer healthcare environment and safeguarding the well-being of healthcare professionals.
It also helps to protect the health of patients by minimizing their exposure to hazardous drugs.
Pharmacy professionals must now adjust compounding policies and procedures in response to updates to USP General Chapters <795> and <797>.
Proposed in 2021, these revisions became official on November 1, 2023 and, according to the USP,
“reflect advancements in science and practice to help ensure quality compounded preparations,
promote public health and protect patients and healthcare workers.”
Specifically, updates to chapters <795> and <797> relate to compounding sterile and nonsterile preparations and address updates to BUDs–or beyond use dates–for these compounds.
In the revised chapters, “the revisions to the BUD limits were established based on a risk-based approach, since it is difficult to predict the stability and microbial susceptibility for all the different types of non-sterile and sterile preparations (e.g., some preparations may degrade more quickly than others and some preparations may be more susceptible to microbial proliferation than others),” according to the USP website.
Patricia Kienle, Director of Accreditation and Medication Safety at Cardinal Health mentioned revisions to chapters <795> and <797> at the 2022 ASHP Summer Meeting and Exhibition. Kienle emphasized that these USP standards represent minimum requirements and encouraged adherence to the best particles for continual improvement.
While understanding the general USP chapters can be challenging, the quality of medicines is important to ensure their integrity, strength and purity for human consumption at a safe level.
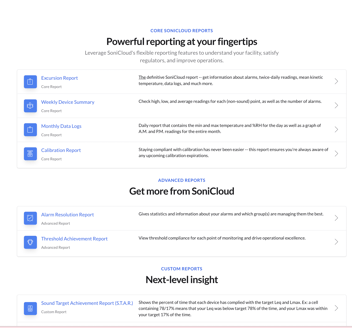
Pharmacy leaders focused on quality and compliance often turn to an environmental monitoring leader like Sonicu for data logging and to reduce the manual labor associated with recording values for compliance reporting.
Chris Peshek, Pharmacy Director, Discount Drug Mart, speaks about how his organization leverages Sonicu for their temperature monitoring requirements.
That is why expert bodies provide strict guidelines – including those provided by the USP chapters – to help ensure that medications placed on shelves are what they claim to be.
Learn more about key USP chapters here.
The recent revisions include nomenclature changes for sterile-to-sterile compounding and impact areas where materials are prepared rather than their ingredients.
They are grouped in the following categories:
-
- Category 1 (low risk) covers the compounding areas where materials are prepared
- Category 2 (medium risk) is for materials prepared in cleanroom suites
- Category 3 covers materials prepared in cleanroom suites using extended beyond-use dates (BUDs), introducing additional personnel and facility monitoring and testing requirements
The importance of USP <800> Compliance
USP chapter <800> delineated protocols for handling Hazardous Drugs in situations where there exists a potential risk of exposure to patients, healthcare workers, and the environment.
This standard is comprehensively relevant to compounding activities as indicated through cross references in USP chapters <795> and <797>, specifically addressing both non-sterile and sterile compounding processes.
In alignment with its intended scope, USP <800> applies only when a practitioner is actively involved in compounding, as per the definitions provided in USP <795> and <797>.
The application of USP <800> is not extended to activities such as administration and dispensing of final dosage forms, which fall outside the purview of USP <795> and <797>.
Consequently, in scenarios where compounding is not part of the process, USP <800> does not govern the handling of Hazardous Drugs.
This ensures that the standard is appropriately directed toward compounding practices, maintaining clarity and relevance in its application.
Regarding repackaging, common concerns do arise as well but Kienle noted that this area is not covered in <795> but rather in a United States Food and Drug Administration guidance document titled “Repackaging of Certain Human Drug Products by Pharmacies and Outsourcing Facilities.”
Kienle noted that, despite not being part of <795>, the listed requirements are enforced by regulations in many states.
Chapter <797> covers repackaging for drugs, diluents, containers and closures, while <800> focuses on protecting workers from hazardous drug contamination during repackaging.
Chapter <795> mainly covers non-sterile compounding, but every state board has different regulations on compounding, so chapter <795> can vary, according to Kienle, who cited the following examples:
-
- Avoid carpeting
- Ensure no other activities are happening during compounding
- A containment ventilated enclosure needs to be certified annually
Compliance in today’s environment can be gained by taking educational courses on USP compliance.
Chapters <795>, <797> and <800> provide the term “designated person” and define it as an individual who oversees training and compliance with policies and procedures.
Kienle also notes the importance of maintaining a checklist and properly training pharmacy staff to execute these skills.
Any organizational practice that is contradictory to this training must be satisfactorily explained, especially to a supervisor or inspector.
It’s essential for everyone who enters the compounding area to receive proper training, not just staff.
Visiting inspectors and supervisors, students in observational capacities, maintenance workers – everyone must adhere to proper procedures.
It's important for organizations to recognize that anyone in the vicinity can impact the operational integrity of the compounding area, and consider what policies and procedures need to be expressed to anyone who isn’t involved in compounding before entering.
Sterile preparations are covered in Chapter <797>, which is where compounding allergenic extracts is covered.
Allergenic extracts need to be prepared in a cleanroom or segregated – not in a regular IV room where they could be contaminated.
It is also stated that they can be prepared in an allergenic extract compounding area, which is a space with a visible perimeter.
It is best to also refer to <797> for the best sterile practices.
Beyond Use Dates (BUDs) outline is also found in <797> but should not be viewed as universal defaults, Kienle said.
The maximum BUDs specified may not be applicable to all preparations, as certain formulations could face stability issues necessitating a shorter duration.
Additionally, it is important to note that transferring compounds from one storage temperature to another can alter the assigned BUD.
Thoughtful consideration of formulation stability and the impact of storage conditions is essential for ensuring the integrity and safety of sterile preparations.
Many pharmacy compliance professionals also rely on a continuous environmental monitoring solution like Sonicu to automate vital compliance activities also related to the USP. Hospital pharmacies like Katherine Shea Bethea rely on Sonicu temperature and environmental monitoring to help automate compliance across their many Illinois locations.
Pharmacies across North America rely on Sonicu for ambient temperature and humidity monitoring as well as air pressure monitoring.
The remote wireless system can alert a pharmacist if conditions are out of specification, and provide the history of the conditions required for state Board of Pharmacy inspections.
Never Alone: Cooperation in Cleanroom Compliance
Relying on a solo expert for USP compliance is not the blueprint for success, cautioned Caryn Belisle, RPh, MBA, the director of pharmacy regulatory compliance, quality and safety at Brigham and Women’s Hospital in Boston.
Belisle emphasized the critical need for a dedicated staff specifically focused on cleanroom compliance.
Proper training of this key component is of the utmost importance, not just for staff but also for those who retrieve these medications off the shelf.
Belisle stressed that expecting a cleanroom manager to look over the entirety of these responsibilities is impractical.
Instead, Belisle recommends having an individual external to the cleanroom’s daily operation solely dedicated to ensuring quality and compliance.
Managing all aspects of compliance can be a significant task for a single person. It is advisable to maintain a separation between quality oversight and operational functions.
The adoption of automation tools like remote wireless monitoring can play a pivotal role in streamlining operations and reducing the burden of compliance reporting.
It all comes down to the safety of staff and production within the cleanroom, so start aiming high for everyone’s safety and recognize the importance of maintaining stringent standards in pharmaceutical compounding operations.