Identifying Open Door Threats in the OR to Reduce Surgical Site Infections

Ann Dine is a program manager for a medtech company and a loving mother of two boys. She was diagnosed with cancer in August and then was scheduled for surgery in October. The procedure was completed as planned, and she went back to work after a few weeks.
But then, three months after her surgery, she caught a fever which was her first sign that she had developed a surgical site infection.
Within six weeks, Ann was forced to undergo five additional surgeries—each one a painful reminder that this wasn’t just about fighting cancer anymore. It was about surviving a mistake that never should have happened in the first place.
For Ann, this was beyond inconvenience; it was a life-altering ordeal. And for the hospital responsible, it was the foundation for a potentially devastating lawsuit.
Operating rooms may be among the most tightly regulated environments in healthcare facilities, but shocking stories like Ann’s demonstrated there’s still work to be done to protect patients during procedures that increase their vulnerability.
Every element must be carefully controlled to minimize the risk of surgical site infections (SSIs) and other complications within the operating room.
Even something as simple as opening a door can compromise the delicate balance of these factors, putting patients at risk of developing a healthcare-associated infection (HAI).
In this article, we’re going to address open door threats in the OR.
Addressing these threats should be a part of every healthcare facility’s surgical site infection prevention strategy. This article will also show how monitoring technologies like Sonicu - which include air pressure differential as well as open door monitoring - play an instrumental role in protecting patients.
The Role of Air Pressure in OR Contamination Risks
Hospitals implement strict environmental controls in ORs to ensure both patient safety and surgical precision. Temperature, humidity, and airflow are meticulously regulated to reduce infection risks and maintain a sterile surgical field.
A closed-door policy is just as critical in preventing contamination as any other infection control measure but is often overlooked as a part of the overall infection prevention strategy.
But why does something as simple as an open door matter?
To understand its impact, we first need to look at how air pressure affects contamination risks in different hospital environments.
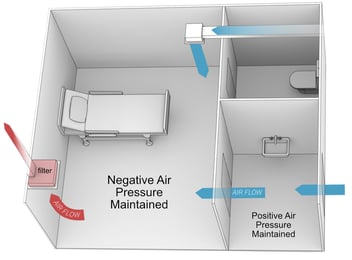
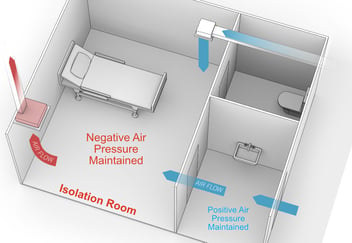
Negative Pressure Rooms
Negative pressure rooms have low air pressure, meaning the existing air in the room feels more stagnant. You may even feel a subtle pull upon entering. This is by design.
These rooms contain airborne contaminants such as bacteria, viruses, and hazardous particles that spread disease.
The following areas would fall into the negative pressure room category:
- Bathrooms
- Soiled laundry areas
- Waiting rooms
- Triage rooms
- Isolation rooms
- Autopsy & dark rooms
- Decontamination areas
Maintaining low pressure keeps contaminated air from leaving whenever someone opens the door, keeping as many bacteria, viruses, or hazardous particles inside as possible.
Positive Pressure Rooms
Positive pressure rooms receive filtered air through specially engineered ventilation systems, strategically located in the ceiling or high on the wall.
This added air is filtered to keep the room sterile for invasive procedures, including surgical operations.
Any “old air” in the room is expelled through an exhaust vent placed low on the floor, directing air flow downward and out.
Whenever the door to a positive pressure room opens, purified air escapes, which increases the chances of airborne contaminants getting inside.
This delicate and precise orchestration between positive and negative pressure is essential, and part of the regulatory standards hospitals are judged against.
Staggering SSI and OR Foot Traffic Statistics
According to the CDC, surveys found an estimated 110,800 SSIs from inpatient surgeries were reported in 2015. By 2023, this number had increased by two percent.
The same CDC study emphasizes the importance of establishing an effective surveillance strategy to detect SSI risks.
Condition-based monitoring and data recording solutions would fall into this category, by offering preventive measures before contaminants can enter the room, such as tracking how often the door opens.
The frequency of door-opening events varies depending on the type of surgery, but according to PubMed, it can range between “19 to 50 events” in an hour.
Studies on OR room traffic discovered that it takes about 20 seconds for the door to the OR to completely close.
When you multiply 20 seconds each time the door opens, the total door ajar time can quickly add up to over 5 minutes. That’s 5 minutes of time for contaminants to enter a positive pressure area.
Despite all the attention COVID forced on this issue, hospitals are still struggling to decrease SSIs while also struggling to maintain discipline on keeping doors closed for non-essential tasks during surgeries.
One-third of all door openings reported are for reasons that were deemed unnecessary.
The Consequences of Inaction Against SSI Prevention
SSIs have a ripple effect across your entire organization.
A single oversight, like an unnecessary open door in the OR, can introduce airborne contaminants that put lives at risk and threaten your hospital’s reputation.
Keeping a controlled OR environment isn’t just about compliance. It’s about protecting patients, staff, and your bottom line.
Like the story of Ann Dine, contracting an SSI in the operating room prolongs patient pain and suffering. Not to mention, the additional stress and financial burden that comes with post-op medical visits.
A patient with an infection may experience delayed recovery, long-term health complications or even deadly consequences.
Not only do patients suffer more from SSIs, your staff does too. Longer patient stays put a strain on hospital resources and medical professionals, resulting in bed shortages and stressed staff.
If an overworked team doesn’t lose staff, those that stay could experience a decrease in overall work performance, which can also pose a risk to patient safety.
SSIs contribute to an alarming rate of extended length of hospital stays, increasing the cost of treatments as much as an extra $37k per patient, according to a PubMed study.
Plus, under CMS’s Hospital-Acquired Condition (HAC) Reduction Program, hospitals with high infection rates receive lower reimbursement payments for procedures.
Depending on your location, if patients acquire an SSI in the OR due to open door contamination, they may have a case to sue for medical malpractice. High reports of SSIs can leave an impression of an unsanitary, negligent environment, which can create a lack of faith in your entire organization.
Legal ramifications can further drain hospital resources and harm a health facility's reputation.
- A surgery center in New Jersey was sued for exposing over 3,000 patients to Hepatitis and HIV. The center paid for the at-risk patients’ blood tests, and now must conduct infection control audits each quarter, and sterilization audits twice a year.
- After what was supposed to be a routine kidney stone surgery, a 46-year-old man developed sepsis post-operation, leading to the double amputation on both of his arms and legs. He now relies on his parents to help him with daily living tasks.
- Three patients developed SSIs after surgeries performed by an orthopedic surgeon. The infections led to severe neurological complications in two patients. The cases were settled for a total of $12.35 million.
It takes years if not decades to build a trusted healthcare brand the likes of Cleveland Clinic or Mayo Clinic, but it can be seriously tarnished in minutes if a patient is injured or even killed by a rogue bacteria that entered an OR through an open door that didn’t need to be opened.
Trust and faith in the healthcare industry is a sensitive matter that’s hard to get back once you’ve lost it.
Hospitals Can’t Afford to Ignore Open Door Threats in the OR
AORN (Association of periOperative Registered Nurses) recommends keeping door openings to an absolute minimum, yet many hospitals lack real-time monitoring to enforce this.
Hospitals that fail to control SSIs don’t just put patients at risk. They also risk losing crucial funding, facing financial penalties, and damaging their reputation.
Strict infection control measures, including maintaining a closed OR environment, are critical to avoiding these costly consequences. Remote wireless environmental monitoring systems like Sonicu can play an essential role in protecting patients, staff, and reputation by delivering real-time and historical data on conditions in the OR.
And a monitoring system can provide the data to help staff recognize beyond a reasonable doubt that excessive open doors impact pressure standards and invite dangerous microbes into what should be a sterile environment.
This case study from UHS South Texas highlights how a facility manager leverages the Sonicu monitoring system to protect his operating rooms from environmental threats.
How to Improve OR Workflow
The average nurse completes over 70 tasks in an hour.
Healthcare workers are already under a lot of pressure to keep patients safe and abide by regulations. But other situations invite scrutiny, especially where patient safety is concerned.
Due to the high-stress nature of the job, there are acceptable reasons for going in and out the door. The following are exceptions that would not be considered an issue, but rather the nature of the job.
Long surgeries, especially those lasting several hours, may require scrub nurses, surgical techs, or other OR staff to take brief breaks or switch shifts.
Alternating personnel, calling in additional support, or leaving to assist in a code blue (cardiac or respiratory emergency) elsewhere in the hospital are all valid reasons to leave the room.
Certain biohazard waste or contaminated instruments must be removed from the OR to avoid excessive clutter and keep the working environment safe and contamination-free.
Transporting patients in and out of the OR requires opening and closing doors, and briefly exposing the sterile field to hallway air. This is of course unavoidable.
If the reason for opening the door doesn’t fall into any of the reasons listed above, it could have been prevented. The key is addressing what you can improve.
Despite careful planning, there may be situations where an unexpected instrument, suture, or piece of equipment is needed mid-procedure.
If these items aren’t readily available inside the OR, a staff member may have to leave the room.
If this turns out to be the underlying cause for your department, then the answer is simple – re-evaluate pre-surgery supply planning and storage.
Medical staff may need to speak to another department for a number of reasons:
- Consulting with pathology, radiology, or anesthesia teams for test results or additional guidance.
- Checking on the availability of intensive care unit (ICU) beds or post-op recovery space.
- Updating family members or coordinating post-op care with nurses outside the OR.
In many instances, it would be safer to use a call-in system to reduce how often staff physically leaves in the middle of an operation. A streamlined communication system will reduce preventable delays in high-stakes environments, where every second matters.
Hospitals that have implemented digital or voice-based communication tools have reported fewer nonessential door openings, improved workflow coordination, and stronger adherence to infection control policies.
Next, consider retraining your staff on the importance of keeping the door closed.
Unnecessary foot traffic could indicate internal issues with the department, such as lax enforcement of work policies.
This would be a good opportunity to address staff behavior and re-educate them on why it is so important to keep the door closed.
Once coaching is complete, establish clear expectations on how unnecessary door-open events will be handled moving forward.
Implement Open/Closed Door Monitoring
Hospitals and their overwhelmed medical staff can’t fix what they don’t track.
The ideal solution to finally start tracking door open rates is to implement a seamless monitoring system designed to fit the unique needs of the OR:
- Real-time alerts when doors open too often.
- Data insights on when unnecessary openings occur, so you can uncover the reason why and address the root cause.
- Improved accountability for staff and better enforcement of policies.
Sonicu is helping some of the finest names in healthcare leverage simple and affordable monitoring to increase awareness about this risk while improving OR patient outcomes.
Save on Cost by Using the Same System for Pressure and Room Condition Monitoring
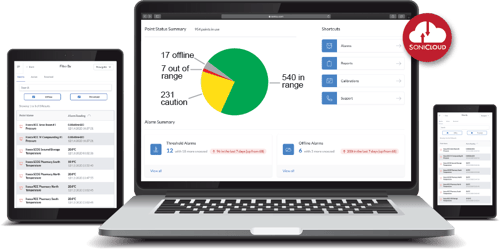
Sonicu offers 24/7 real-time monitoring and automated data recording in a secure, cloud-based integration system you can access on a phone, tablet, or computer.
This all-in-one solution eliminates the need for multiple monitoring solutions, saving both time and operational costs while ensuring compliance with hospital safety standards.
- Room Pressure Monitoring: Prevent cross-contamination between positive and negative pressure rooms with a monitoring system pre-set with the correct air pressure differential thresholds.
- Room Conditions Monitoring: Track both the temperature and humidity levels to prevent microbial growth and maintain a comfortable working environment for your hardworking surgical team.
- Open/Close Door Monitoring: Know when the door opens to help identify unnecessary foot traffic in and out of the OR and minimize open door contamination risks.
Hendricks Regional Hospital – one of Sonicu’s largest clients in the healthcare space – utilizes Sonicu system-wide for all its monitoring needs.
By combining air pressure, environmental, and door closure monitoring in a single, scalable solution, hospitals can streamline infection control, reduce human error, and enhance patient safety—all while cutting costs on multiple, disjointed monitoring systems.
Sonicu Monitoring is Trusted By Hundreds of Hospitals
SoniCloud, our cloud-based platform, is built with simplicity, security, speed, reliability, and scalability in mind.
You can review and manage points of monitoring through the SoniCloud platform, and get instant alarms via email, text message, phone call, or push notification through the mobile app.
"SNAP" Calibration Services - Sonicu’s SNAP Calibration Program is an annual service designed to ensure your sensors remain compliant with National Institute of Standards and Technology (NIST) standards all year long.
Sonicu’s US-based Customer Success & Tech Support teams are here to assist you with any questions or concerns regarding setting or troubleshooting your OR monitoring system.
Outside of regular support hours, you’ll have instant access to Sonicu’s help center page with answers to common troubleshooting questions. Complete with video tutorials and step-by-step guides.
Simplify Operating Room Monitoring with Sonicu
The best time to start tracking door swings in the OR was years ago. The second best time to start is now.
Discover how Sonicu can streamline your operation room door monitoring process, and help you keep the door closed on contamination risks.